Original paper here
What is this study about
- Authors hypothesized that given intramuscularly, Ketamine would work quicker (and safer) when compare to traditional benzodiazepine and antipsychotic medication.
- This is a RCT based on ED patients at a Canadian hospital in Vancouver
- Although ED diagnosis is not stated, the age of these patients and prior history suggest primary mental health disorder and drug/ alcohol plays a big role in their acute agitated state.
Bottom line
- Study is underpowered due to COVID-19 outbreak. In this RCT ketamine is about 3x faster to produce clinical effect compared to study drug. Lack of statistical evidence due to underpowered study, and lack of reporting of subsequent outcome (need for redosing, emergent phenomenon) limits the application of this study to day-to-day clinical practice.
- Choice of chemical sedation for acutely agitated patient in the ED, is still determined by individual clinician preference and familiarity.
Study design
- Parallel-arm 1:1 randomized trial at ED of St. Paul’s Hospital
- Research assistants received standard video and lecture training on trial protocols and assessments
- Of the 80 people included in the study
-
40 patient receiving 5mg/kg IM (max 4mls per syringe allowing multiple syringes)
vs
40 patient receiving 5mg IM midazolam + 5mg IM haloperidol (single syringe)
- To achieve 80% power with a harm reduction of 1.56, the study would have required 83 patients in each group, for a total of 166 patients
Outcome measurement
- Primary end point is, in minutes, from drug administration to RASS ≤ -1
- Secondary outcomes were:
- Need for rescue medication – benzodiazepines, antipsychotics or other sedatives (at treating clinician’s discretion)
- adverse events
- Occurrence of neuroleptic malignant syndrome within 72 hrs (chart review, records and telephone follow-up)
- Assistants prospectively record:
- RASS continuously at 5 mins interval until primary end-point (
- adverse events until discharge from ED
- Principle investigator review safety data, and 2 independent emergency physicians not involved with study review any potential serious adverse events
Study population
- Patient presenting to this ED between 8am and midnight (when study staff is available) between June 30, 2018, and March 13, 2020
- 19 to 60 year old with severe psychomotor agitation measured by Richmond Agitation Score (RASS) ≥ +3
- 308 pt was eligible during study period. 278 was excluded resulting in 80 being randomized (1 pt in control arm excluded due to screening error)
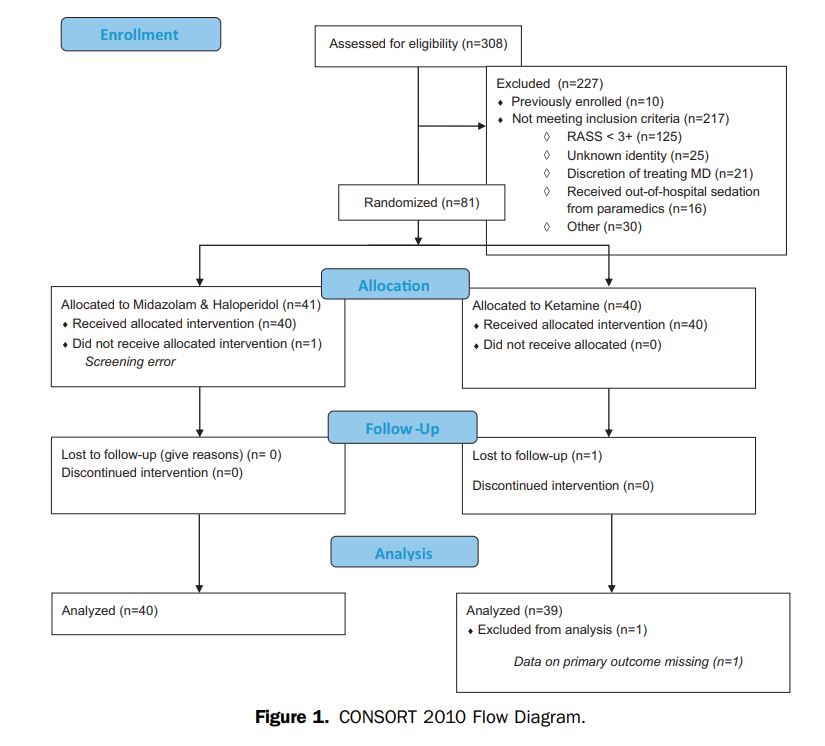
- Exclusion criteria in figure 1
- Important exclusion criteria is younger and older patient, patient with multiple medical or airway co-morbidity.
- Pt who received out-of-hospital sedation from paramedics also excluded, pt with unknown identify, pt with RASS ≤ 3 also excluded
Background characteristic
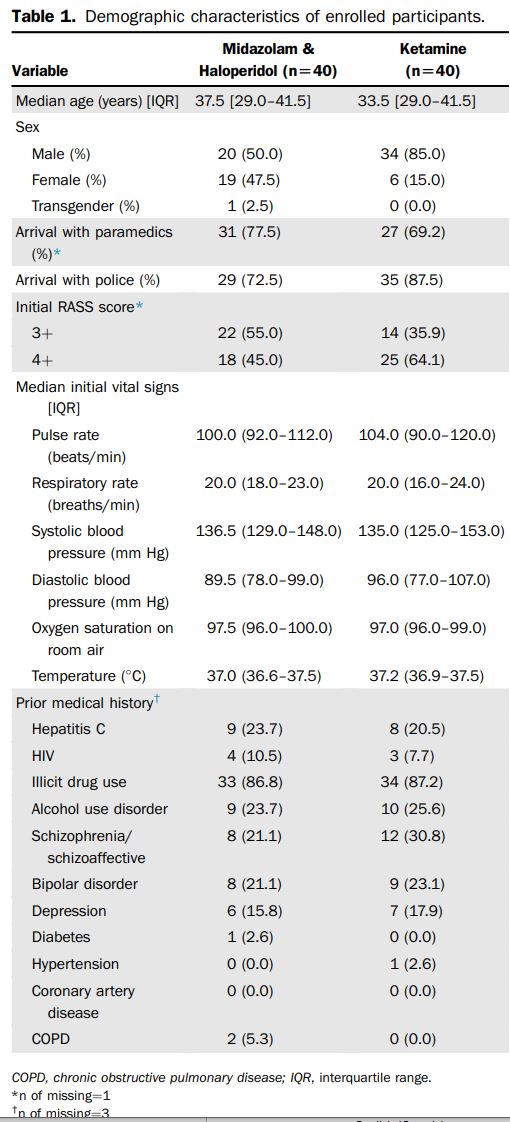
- Patient background characteristic in both arms (table 1) fairly equal. Almost 90% have prior history of illicit drug use, in addition to 25% with/ concurrent hx of alcohol use disorder and mental health disorder.
- Mean age of patient is 35 years old
- However, there is some major major difference in both group which may actually favor study conclusion (more likely true positive study even though it is a small study):
- There is 34 male pt receiving ketamine compared to 20 female receiving midazolam/ haloperidol.
- More patient in ketamine arm have RASS score ≥ 4+
Statistical analysis
- Intention-to-treat basis
- SAS was used to statistical analysis
- P values were reported and all tests were 2-sided
Result
- The median time to sedation was 14.7 minutes for the haloperidol/midazolam group and 5.8 minutes for the ketamine group, with a difference of 8.8 minutes.
- Adjusted Cox proportional model analysis favored the ketamine arm (hazard ratio 2.43, 95% CI 1.43 to 4.12).
- Of the patients who received ketamine, 5 reported adverse effects.
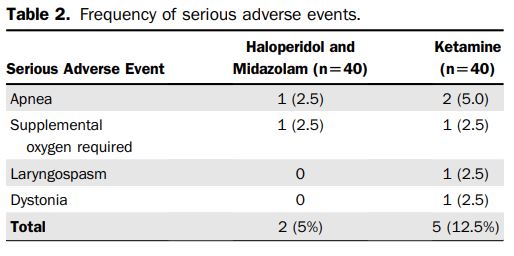
- 5 (12.5%) patients in the ketamine arm vs 2 (5.0%) patients in the midazolam and haloperidol arm experienced serious adverse events (difference 7.5% [95% CI -4.8% to 19.8%]). Adverse effects were rare and not serious.
- The 1 patient who developed laryngospasm, condition self-resolved and did not require intubation.
Conclusion
- Author concluded that in ED patients with severe agitation, intramuscular ketamine provided significantly shorter time to adequate sedation
than a combination of intramuscular midazolam and haloperidol.
Discussion
- Rapid behavioral control for patient and staff safety is a controlled procedure often carried in the emergency department, when patient presented with severe psychomotor agitation
- These patient are often undifferentiated and carries risk of allergy, airway risk, aspiration risk etc.
- Midazolam, haloperidol, ketamine are all commonly used medication for this purpose
- Each of above have its own risk and challenges
- Benzodiazepines: respiratory depression, oxygen desaturation, needing airway interventions
- Antipsychotic: dystonia, akathisia, parkinsonism, neuroleptic malignant syndrome
- Ketamine: Bronchospasm, re-emergent phenomenon, repeat dosing can be difficult especially when compared to benzodiazepines which is predictable
- Pre hospital use of ketamine for sedation has been studied
- Lack of high quality evidence for ED, hospital use of ketamine especially intra muscular route.
- Unfortunately, this study did not answer the question. What it does is that it adds to the growing number of evidence, allowing for a big meta analysis or a later RCT to support (or vice-versa) the use of IM ketamine for this purpose.
- Clinical effect of IV administration of midazolam and haloperidol is more rapid as IV ketamine and titratable. Unless IV access is not possible or at discretion of treating clinician, IM ketamine may not be relevant in daily practice.
- A limitation of the study is that outcomes after the 30 minutes of observation are not reported. This information would have been valuable, because giving ketamine to sedate acutely agitated psychiatric patients carries a risk of emergent reaction.
- Administration of multiple syringes of IM medication increased risk of needle stick injury, drug administration error, risk of infection and bleeding.
- Finally, the dose of control drug are relatively small for this purpose and not usually administered in this combination in reviewer’s experience (i.e. usually 10mg IM midazolam, obtaining IV and baseline ECG before 5mg IV droperidol), but not unreasonable.
- For reviewer, this small study demonstrated:
- A safe IM dose i.e. 5mg/kg (if IM route required)
- The time to effective sedation is 6 mins
- Laryngospasm is uncommon and self limiting (in this small sample size)
