A 42 year old man has presented with a self limiting episode of palpitations this morning.
He noticed on his apple watch that his HR was recording as 190 bpm. On assessment he is now asymptomatic and observations are stable. He has no other PMH.
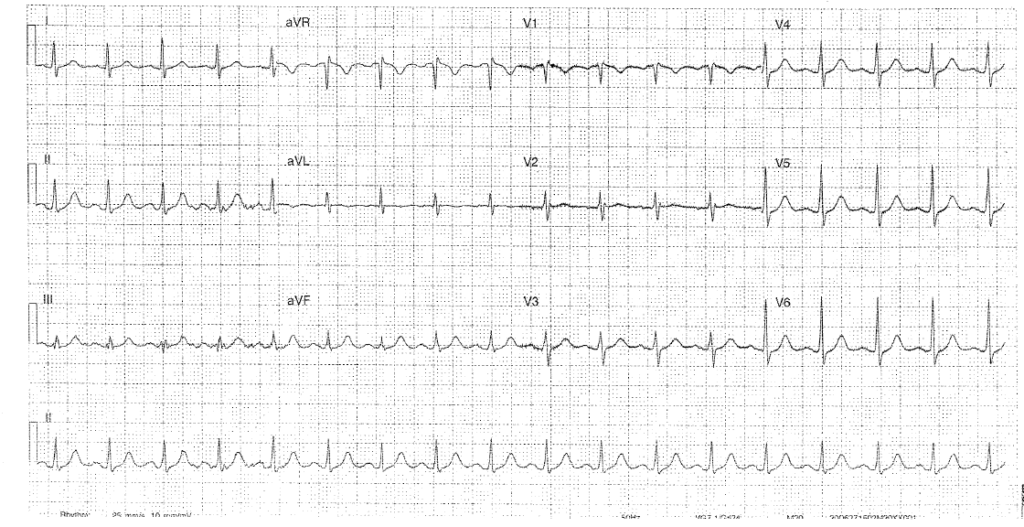
His ECG is as below:
Interpretation:
- Rate: 108
- Rhythm: Sinus tachycardia
- Axis: 0-90
- Morphology: bifid p waves, TWI aVL, of note coved STE <1mm V1 consistent with a Brugada Type 3 pattern
- Intervals: PR 160 QRS 90 QTc 390
- Summary:
Further information / history required:
- Heritage / descent
- FHx of sudden cardiac death
- Previous history of syncope, seizure like event, VF or VT.
- B/g of nocturnal agonal respiration
- For this patient he was from Singapore and had a FHx of sudden death in both his maternal Aunt and Grandfather.
Management:
- Resus: no ABC issues
- Telemetry
- Check electrolytes in context of tachycardic episode
- Risk of dysrythymia in Brugada Type 1 patients- therefore admit for ICD
- There is controversy re Brugada type 2 and 3 management – could also consider d/c with OP EPS and cardiology F/u
- The other treatment option consists of Na channel blockade provocation in Brugada 2 and 3 patients (which may convert this non diagnostic change into a type 1 brugada ECG change BUT sensitivity of this is not known) – obviously this needs to take place in a safe setting as Ventricular dysrthymia may be precipitated
Discussion:
- Inherited arrhythmogenic condition with a 10% per year mortality risk
- 30% patient have a genetic mutation in cardiac Na channels
- Commonly seen in people of SE Asian descent
- And in patient >40 (seen in ages 20-55 classically)
- May also present asymptomatic on incidental ECG
- 3 ECG patterns
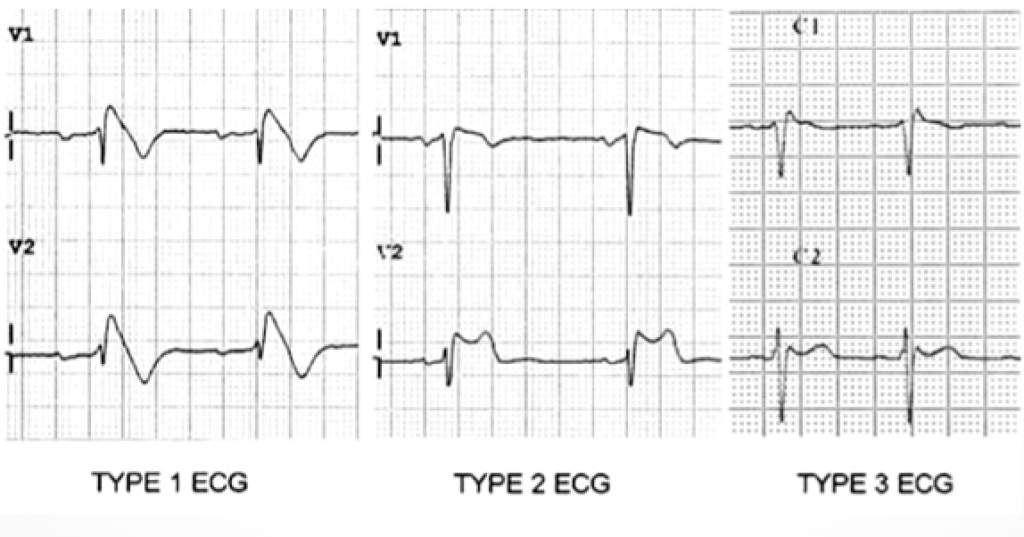
Type 1: coved STE >2mm in >1 of V1-V3 at J point, followed by inverted T wave (this is the only ECG change that is potentially diagnostic of Brugada)
Type 2: Saddleback ST segment with >2mm J point elevation, and +ve or biphasic T waves
Type 3: coved or saddleback STE <2mm
Tip – increase ECG sensitivity by putting leads in V1 and 2 in 2nd (not 4th ) intercostal space
- Diagnosis:
ECG + at least one clinical criteria
(+ve family hx, arrhythmia related symptoms – syncope, seizure like event, nocturnal agonal respirations, VF or VT documented)
Further reading:
Textbook:
Chan TC, Brady WJ, Harrigan RA, Ornato JP, Rosen P. ECG in Emergency Medicine and Acute Care. Elsevier Mosby 2005.
Online:
For a case of Brugada type changes as seen in Carbamazepine use see the ECG case below: