A 50 year old female presents to ED complaining of chest pain. The patient is well known to the department, with frequent presentations with chest pain.
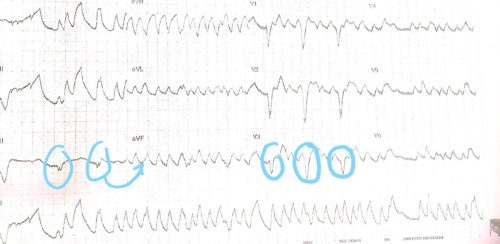
Recent MPS shows mild reversible inferior changes, which is unchanged from 2 years ago. While the patient is awaiting doctor assessment the following rhythm is noted on the monitor and a 12 lead ECG is then captured:
- Describe and interpret the ECG
- How would you approach the assessment and management of this patient
Answer
Rhythm Strip: Wide complex tachycardia PVT/VF
12 Lead ECG:
Rate: 75 beats per minute
Rhythm:Appears regular, if QRS is mapped out backwards from leads V1/V2/V3. No P waves seen due to marked artifact
Axis:Unable to determine due to marked artifact
Intervals
- PR: No P waves seen
- QRS: 200ms
- QT: Unable to determine
Additional: Normal ventricular complexes with LBBB morphology noted in the chest leads. (The patients baseline ECG is LBBB) These complexes can be mapped out to notching within the “PVT” in the limb leads.
The 12 lead ECG shows that the initial rhythm strip is most likely artifact.
The following features suggest that a dysrhythmia is likely artifact:
- lack of symptoms or haemodynamic instability during the event
- appearance of normal ventricular complexes amongst the dysrhythmic beats
- body movement at time of abnormal tracing
- tracing baseline instability during and immediately after the apparent dysrhythmia
- visible notching in the complexes of the dysrhythmia that line up with the ventricular complexes that precede and follow the apparent rhythm disturbance
On initial rhythm strip the patient is thought to be in PVT, therefore assessment would include determining if the patient has a pulse, are they alert, and what is their blood pressure and do they have other concerning features like chest pain or CCF.
If time and stability of the patient allows, a 12 lead ECG should be done to further define the rhythm and exclude artifact, as in this case.
If the patient is unstable or 12 lead confirms PVT (non torsades) management would include shock, medication – betablockers or amiodarone , and seeking and treating underlying cause eg ACS/Brugada
References:
Chan TC, Brady WJ, Harrigam RA, Ornato JP, Rosen P, 2005, ECG in Emergency Medicine and Acute Care, Elsevier Mosby, USA