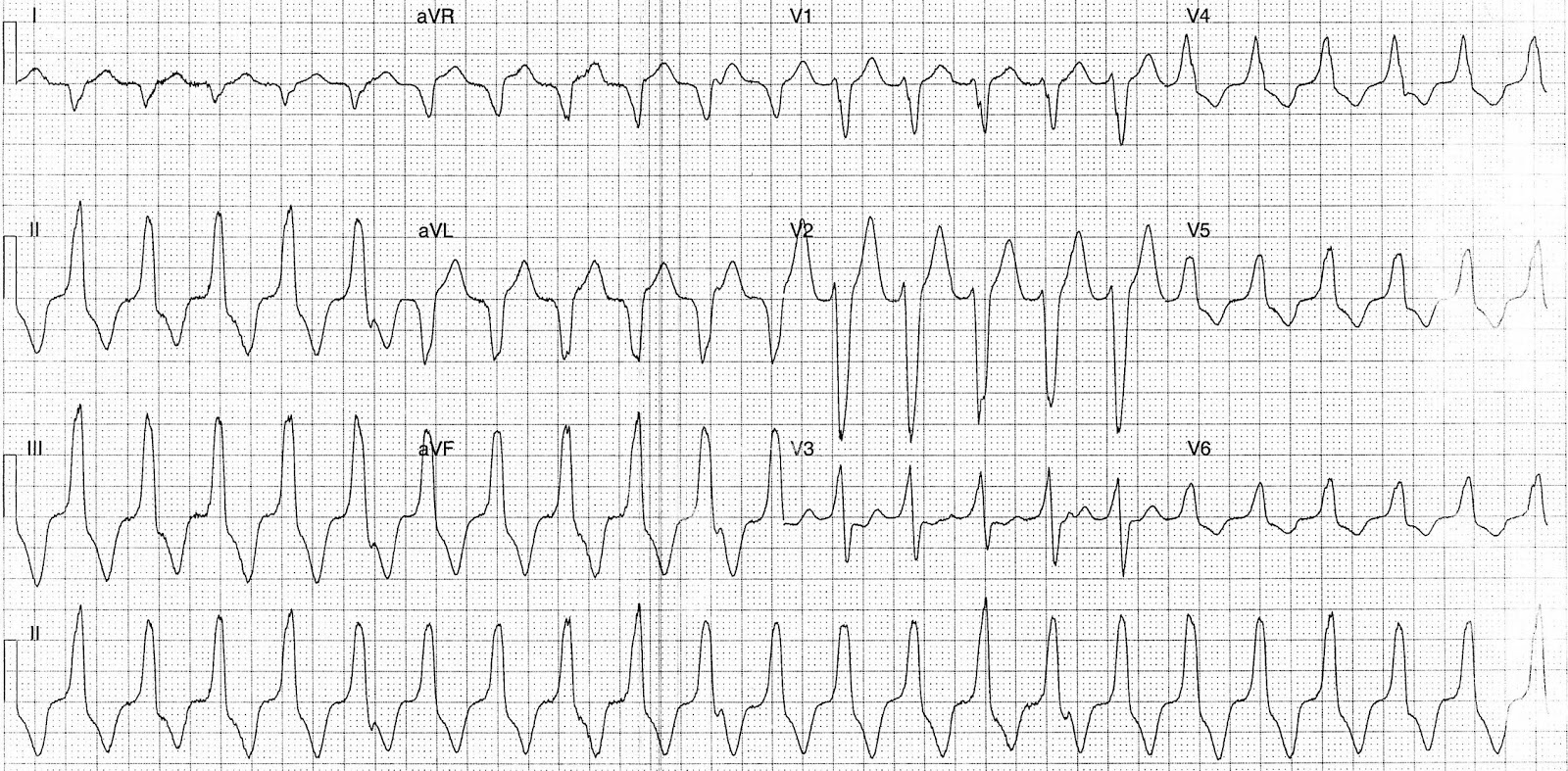
33 y/o female presented with 6 hours history of palpitations and dyspnea. She denied any chest pain. Her Blood pressure is normal.
Rate:
- 132 bpm
Rhythm:
- Regular
- AV dissociation
Axis:
- Inferior (Near isoelectric lead I with positive lead aVF)
Intervals:
QRS – Prolonged
Additional:
- LBBB Morphology
- Nil capture beats
- Nil fusion beats
Interpretation:
Wide complex tachycardia.
LBBB Morphology with inferior axis and features supportive of VT (AV dissociation)
The combination of LBBB morphology and inferior/right axis deviation is consistent with Right Ventricular Outflow Tract Tachycardia (RVOT). This is a type of monomorphic VT originating from the right outflow tract or tricuspid annulus it is commonly seen in structurally normal hearts and is usually hemodynamically well tolerated.
Clinical implications
- RVOT tachycardia can be difficult to distinguish from SVT with LBBB
- Inferior axis (+90 degrees) is usually the most differentiating feature, but other features of VT such as AV dissociation may be present
Treatment:
- Acute termination of idiopathic RVOT tachycardia in a stable patient can be achieved by vagal manoeuvres or adenosine (6mg up to 24mg)
- IV verapamil is an alternative if the patient has an adequate blood pressure reserve.
RVOT can also be seen in arrhythmogenic right ventricular dysplasia (ARVD). RVOT tachycardia in ARVD does not terminate with adenosine.
ARVD is a genetic disorder of the myocardium in which there is fatty infiltration of the right ventricular free wall, and accounts for up to 10% of sudden cardiac death in individuals under 65 years of age. Affected individuals often present with exercise-induced episodes of VT accompanied by LBBB morphology.
Differentiation between idiopathic RVOT tachycardia and that caused by ARVD can be difficult and may rely on previous ECG findings as well as family history.
Closure:
This patient reverted following vagal maneuvers.
ECG was taken from Dr. J Larkin ECG of the week Blog.
Additional reading/Reference: