83 years old male has been brought to ED by his wife with fever, confusion and epigastric pain. He was seen by GP 2 days ago with fever and was diagnosed as having LRTI ( no antibiotics given ). He has history of T2DM, HTN, and cholecystectomy 10 years ago.
His vitals are : HR 115, BP 105/70, temp 39. RR 22, sats 95 RA, GCS 14 ( confused). abdomen soft, mildly tender RUQ, and epigastrium.
Patient had VBG which was consistent with HAGMA . Electrolytes were normal, lactate 2.5, and Creatinine 125. Patient had other blood tests done as part of workup and LFTs came back as following.
Bilirubin 67 (< 21)
ALP 320 ( 30 -110)
GGT 368 ( < 41)
ALT 248 ( < 36)
Q1: Interpret above Liver function tests ?
2. What is the most likely diagnosis with this clinical picture and LFTs?
3. What are the important considerations in management of this patient ?
Answers: 1 . There is hyperbilirubinemia, raised ALP ( almost 3 times the normal limit), raised ALT ( almost 10 fold increase and raised GGT ). This is consistent with “cholestasis” or obstructive picture. ALT is a marker of hepatocellular damage, where as ALP is a marker of “cholestasis/ obstruction. GGT is most sensitive of all, and will be raised in most of hepatobiliary insults but not very specific. A general guide for ALT/ ALP comparison is: A greater than 10-fold increase in ALT and a less than 3 – fold increased in ALP suggests predominantly hepatocellular damage. Where as A less than 10-fold increase in ALT and more than 3-fold increase in ALP suggests cholestasis.
Remember: it is possible to have mixed picture ( obstructive and hepatocellular damage ) in cholangitis because of hepatic damage secondary to obstruction. Diagnosis is mostly guided by whole clinical picture i.e fever, jaundice, tenderness, and then abnormal LFTs and imaging.
Answer: 2 . The most likely diagnosis is “Acute Cholangitis “. Other differentials would be hepatitis, septic shock. The classic Charcot’s triade of fever, RUQ tenderness, and jaundice is present in 50-70 percent of patients with cholangitis. Any condition that leads to obstruction of bile in CBD ( stones, stricture, malignancy, parasitic infestation,external compression from pancreas will lead to stasis, trans mural migration of bacteria in bile and ascending of infection towards hepatic channels. Fever is present in 90 % of cases, Abdominal pain, jaundice are present in about 60 percent of cases. Hence many patients especially elderly do not have typical symptoms of cholangitis. Bilirubin is elevated in 88-100 % of times, ALP rises in 78 % of times. There will be leucocytosis and raised CRP.
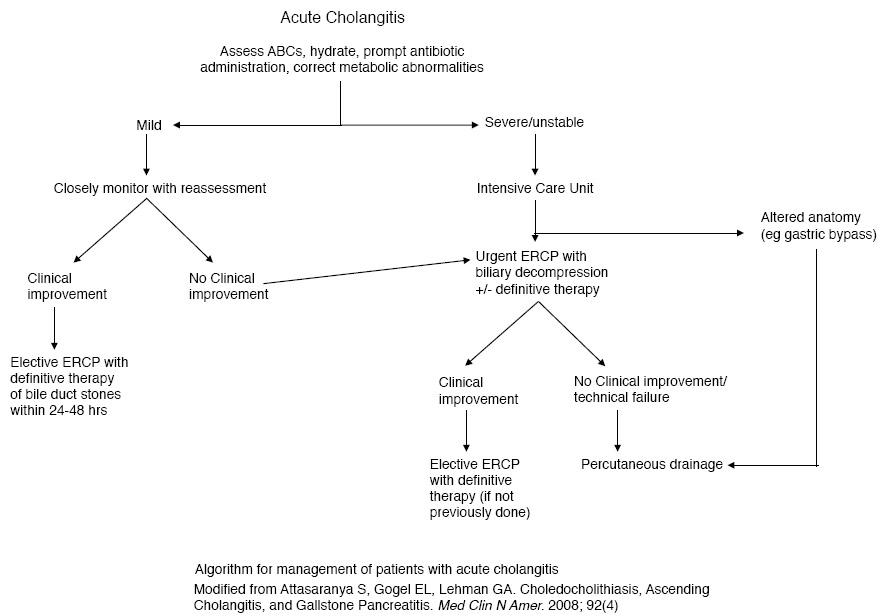
Answer: 3. Patients with acute cholangitis can be very sick, and need attention to airway, breathing, circulation . Early broad spectrum antibiotics, fluid resuscitation and ongoing close monitoring. If patients are septic or unwell they need urgent ERCP, if mild cholangitis 70-80 % settle with medical management and then need ERCP within 24-48 hours. ERCP is both diagnostic and therapeutic. Biliary USG is first modality of imaging if patient is stable ( not very sensitive to distal CBD stones), CT abdomen more sensitive for picking up cholangitic changes and supports diagnosis. MRCP is highly sensitive for cholangitis diagnosis and is suitable for stable patients. If patient is unwell ERCP is the modality of choice for both diagnosis and treatment.