Your patient is a 2 yo boy brought in by his mother after he choked on a peanut. This is his CXR.
Airway foreign bodies
3 types of obstruction once object lodged in the airway:
Bypass valve obstruction
– air passes in and out
– no radiographic changes
– may cause no symptoms
Check valve obstruction
– exhalation around object prevented
– obstructive emphysema results
Stop valve obstruction
– both inspiration and expiration blocked
– distal atelectasis results
– pneumonitis may occur
Clinical exam:
– brassy cough
– voice changes
– bi-directional stridor (during inspiration + expiration)
– unilaterally decreased breath sounds
– localised wheezing
– signs of respiratory failure – tachy or bradypnoea (for age) / tachycardia progressing to bradycardia / initial increased work of breathing, which can progress to decreased and inadequate work of breathing
– complete airway obstruction and asphyxia with cyanosis, stridor, altered mental state followed by respiratory arrest can result from a large object lodged in the trachea or larynx
CXR:
– radio-opaque object seen on chest x-ray
– air trapping during inspiration and expiration (suggestive of main bronchus obstruction)
– atelectasis
The sensitivity of chest x-ray performed in the emergency department for foreign body aspiration was found to be only 22.6% with false-negative rates of 5% to 30% in children.
So a NORMAL chest Xray DOES NOT rule out an airway foreign body.
If there is clinical suspicion that the object might be lodged in the upper airway, a lateral soft tissue Xray of the neck might be helpful.
Children with suspected inhaled foreign body should NEVER be held down for imaging as this might dislodge it and cause complete obstruction.
Children who are in extremis should NEVER be sent to Radiology for imaging. Airway should be managed first, then they can have portable CXR, but this should not delay transfer to PMH for bronchoscopy by ENT or Respiratory medicine team.
Which children with suspected inhaled FB should be referred to the Respiratory team at PMH for bronchoscopy?
“2 of the 3 rule”
1. history suggestive of aspiration
2. examination findings compatible with an inhaled FB
3. radiological findings compatible with an inhaled FB
In “low risk” children who are discharged home from ED, parents should be advised to return to ED if the child has ongoing cough, noisy breathing or recurrent chest infections.
Coming back to our patient, there is air trapping on the left side suggestive of left main bronchus obstruction and no foreign body is visualised (only 20-23% of inhaled foreign bodies are radioopaque)!


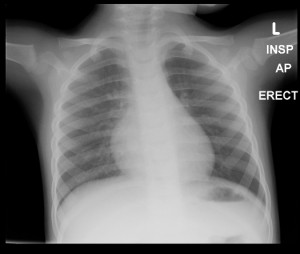
Great work with the daily pearls Ioana!! Interesting that we went with insp/exp films in this 2 year child. It might be worth noting that a lateral decubitus film can be useful in kids who aren’t able to comply with insp/exp films.
Thanks Simon. And thanks for mentioning the lateral decubitus film.
This was not my patient, but I guess it’s not just the age – you might get a 5 yo who will not comply with insp / exp films – and it depends on the parents and the radiographer as well. But you can always try.
Just a quick note: with gas trapping, the expiratory radiograph is more useful, as the non-obstructed lung will collapse and become denser/whiter, whereas the obstructed lung will remain aerated due to gas trapping, thus remaining blacker. While this can be appreciated on the inspiration radiograph, the expiratory radiograph accentuates the differential lucency of the two lungs.
Ken (radiol reg)
Thanks Ken. That’s very true, the only problem is that it can be quite subtle and I find it a bit easier to see the difference between the 2 lung fields on the expiratory film after looking at the inspiratory film where they look pretty much the same.
Agreed. Comparison between insp and exp is always preferable, if both are available.