The ECG below is from a 46 year old lady who has presented to ED at 7pm after experiencing palpitations since 2am that day, but otherwise feels well.
She has had 5 episodes of similar over the last 15 years but has never presented for investigation before. Her PMH includes asthma, sleep apnoea, oesophageal spasm, Von Willebrands disease and depression. She takes Salbutamol PRN as her only medication. She is also an ex-IVDU with last injected use 16 years ago. She continues to smoke Meth and last did so yesterday evening. She also regularly smokes THC.
Her observations are BP 119/76, RR 16, Sats 100% air, T 36.8.
On examination she has a clear chest, HS are normal with no murmurs and there are no peripheral stigmata of Infective Endocarditis.
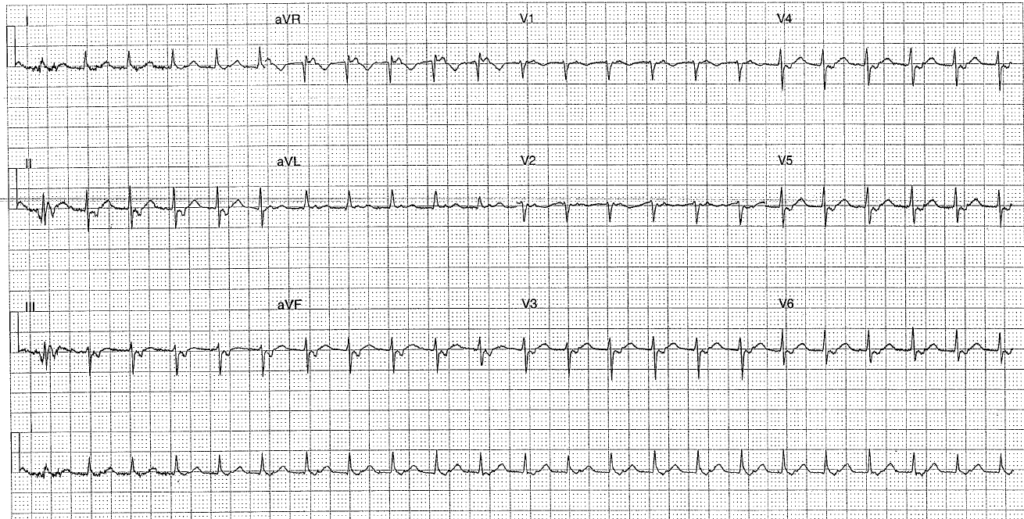
This is her ECG:
Interpretation:
- Rate: 138
- Rhythm: Regular
- Axis: Normal (0-90)
- P axis: 180- negative 90 (extreme axis)
- Morphology: narrow complex tachycardia, retrograde p waves (largely negative except in leads I, aVL, aVR, V1 and V2), flat T wave V2
- Intervals: PR not applicable (retrograde) QRS <120
- Summary: Regular narrow complex tachycardia with retrograde p waves (See discussion below) – a type of supra ventricular tachycardia.
Discussion:
So what kind of SVT is this? Supraventricular tachycardia (SVT) is a tachycardia which has its electrical start point arising above the bundle of His and causing heart rates of greater than 100 beats per minute.
The commonest types of paroxysmal SVT are: atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reciprocating tachycardia (AVRT), and atrial tachycardia (AT – eg Atrial flutter and multifocal atrial tachycardia).
AVNRT is the commonest SVT in adults with structurally normal hearts. It is more common in woman and typically paroxysmal. Rate normally lies between 140-280 bpm and is regular. It may cease spontaneously, and even if this is not the case is often well tolerated. Pathophysiology lies in a re-entry pathway that lies in or around the AVN. This circuit consists of a slow and fast pathway. The commonest AVNRT is a Slow-Fast AVNRT where the slow AVN pathway provides anterograde conduction and the fast pathway is retrogradely conducted.This means the p wave is retrogradely seen in the ECG, hiding in the QRS complex or seen at the end of the QRS as a pseudo r’ or S wave. In contrast the uncommon Fast-Slow AVNRT is anterogradely conducted down the Fast AV node pathway and retrogradely via the Slow AV nodal pathway. This gives a retrograde p as a QRS-p-T complex as seen in this case.
Just for confusions sake there is also the atypical Slow-Slow AVNRT (which I will not discuss here but will instead reference to the Life in the Fast line article linked below if you wish to read up further on this)
AVRT in contrast is caused by a re-entry circuit within an accessory pathway (where the ventricles are activated early by a pathway that bypasses the AV node) AVRT can be divided according to the direction of the re-entry (Orthodromic is clockwise, Antidromic is counter-clockwise) Both tend to have a rate of between 200-300 so not likely with this case.
Junctional tachycardia: a tachyarrhythmia where the rate of an AV junctional pacemaker (ie close to Bundle of His and thus producing a normal narrow complex) is faster than the SAN. Junctional rhythms can either be Automatic (where the automaticity of the AVN increases) or Re-entrant (where there is a re-entry loop at the AVN eg in AVNRT). This ECG could be an example of junctional tachycardia given that the QRS is narrow and there are retrograde p waves which can be a common feature. The p wave inversion in the inferior leads here indicates a non-sinus origin of the P waves
In terms of other SVTs:there are no flutter waves to indicate Atrial flutter.
So….does working out the exact classification of dysrhythmia alter her management? Not really……
Management
- If in doubt and the patient is unstable cardiovert
- Use of vagal manoeuvres to stimulate the vagus nerve can stop some SVTs inc AVNRT.
- Adenosine works to block the AVN and can be successful in both junctional tachycardia and AVNRT (note this won’t work with AT because it is an atrioventricular nodal-independent SVT)
Clinical Closure:
Given the history of drug use she was discussed with the Cardiology team in case her case was consistent with Infective Endocarditis (which can cause junctional tachycardia by affecting the Mitral or Aortic valve and cause oedema affecting the AV node). After their review, where she had remained well and stable with bloods that did not support an infective process they were confident she did not have infective endocarditis and were happy to proceed with a trial of adenosine after which she reverted to NSR.
Further Reading – Textbook:
Chan TC, Brady WJ, Harrigan RA, Ornato JP, Rosen P. ECG in Emergency Medicine and Acute Care. Elsevier Mosby 2005.
Further Reading – Online:
And for a far more eloquent and diagmatic description than I can give see the You Tube tutorial from open.osmosis.org via Tài Nguyễn Nhật below: