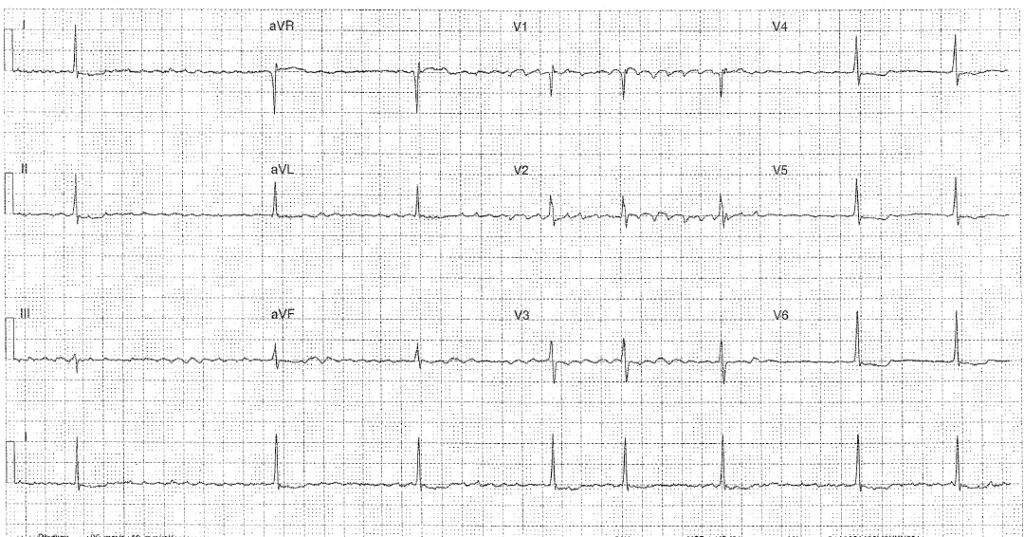
The following ECG is from an 83 year old lady who has presented with new renal impairment following a fall (Na 134 K5.4 Ur 12.4 Cr 164 from a baseline of 110).
Interpretation
- Rate: 48
- Rhythm: Atrial fibrillation
- Axis: Normal 0-90
- Morphology: Downsloping segments V4-6
- Intervals: QRS 80 QTc 193 (Bazzett) 200 (Fredericia)
- Summary: In a patient with slow AF and renal impairment we must always consider Digoxin toxicity.
Discussion
Why do we use digoxin and how does it work:
- Positive ionotrope
- Affect on Na-Ca exchanger cause Ca2+ to increas, resulting in stronger contractions
- Negative chronotrope
- Increased vagus nerve activity causing lowered heart rate by reducing automaticity at the sino-atrial node and slowing conduction across the atrioventricular node
The Digoxin effect seen in this ECG show that the patient is taking Digoxin rather than being a marker of toxicity
- Downsloping ST depression
- T wave changes: flattened, inverted, biphasic
- QTc shortening
- ?J point depression
Other ECG features that may be seen
- U waves
- PR prolongation
Why do we see ECG change in the context of digoxin?
- The refractory periods of both atria and ventricles shorten
- This shortens QTc
- Secondary depolarisation changes which results in the change to ST segments, T and u waves.
Typical ECG in chronic toxicity
There is a clinical difference between an acute (eg overdose) case of toxicity vs chronic toxicity which is more commonly seen in elderly patients with renal impairment, especially in the context of an acute illness. Patients with chronic toxicity may develop cardiovascular and GI symptoms as well as changes in vision such as xanthopsia and chromatopsia
- AV blocks due to reduced AV conduction
- Bradycardia or slow AF
- Regularised AF – AF with CHB
- Ventricular Ecoptics – including ventricular bigeminy or trigemini
- Supraventricular Tachycardias due to increased automaticity
Clinical Symptoms in Toxicity
- CVS: syncope, palpitations
- GI: diarrhoea, nausea or vomiting
- CNS: fatigue or confusion
- Visual: abnormal colouration – yellow / green, halo vision, blurring
Treatment
- Digibind
- Correct any hyperkalaemia
- Bradycardia: atropine and pacing rarely effective, adrenaline may worsen symptoms
- Consider dialysis when appropriate in context of renal failure
Further Reading – Textbook:
Chan TC, Brady WJ, Harrigan RA, Ornato JP, Rosen P. ECG in Emergency Medicine and Acute Care. Elsevier Mosby 2005.